info
Monday, 30 April 2018
Epidermal Choristoma Presenting as an Enlarging Tongue Mass
Epidermalchoristoma is an extremely rare entity characterized by histologically
normal-appearing skin with associated hair follicles, sebaceous glands, and
adnexa in an abnormal location. When localized to the oral cavity, this lesion
presents most-commonly as an asymptomatic hyper pigmented macule or patch on
the lingual dorsum of a male patient. Herein, we present an unusual case of an
epidermal choristoma presenting as an acutely infected mass of the deep
anterior tongue in a teenage female.
Choristomas are a developmental abnormality characterized by
the proliferation of histologically normal tissue in an ectopic location.
Choristomas of the head and neck have been noted in the tongue floor of
mouth nasopharynx pharynx hypopharynx and submandibular regions and are clinically important lesions as they may present as a cause of
airway obstruction or feeding/ swallowing difficulties, especially in the
pediatric population. In the oral cavity, heterotopic tissue consistent with
choristoma has been reported with otherwise histologically-normal salivary
gland, cartilaginous, osseous, thyroid, sebaceous, glial, gastric mucosa, and
epidermal tissues although cartilaginous, osseous, and lingual thyroid
choristomas are relatively more common. “Epidermal choristoma” or
“cutaneous choristoma” is defined by the presence of stratified squamous
epithelium (epidermis) with associated adnexal structures including sebaceous
glands, apocrine glands, and hair follicles. Epidermal choristoma is a very
rare lesion of the oral cavity, with only five reported examples in the
literature to date. All reported cases have occurred in males, with the
majority presenting as a hyper pigmented macule or plaque (80%), most commonly
of the dorsal tongue. Follicular choristoma appear to be a related lesion
defined by pigmented epidermis, sebaceous glands, sweat glands, and mature hair
follicles with the additional finding of keratin-containing cysts. To date,
there are two cases of follicular choristoma reported in the English language
literature. Herein, we report a unique example of an epidermal choristoma
presenting as an infected tongue mass in a female teenager.
A 14-year-old female with no significant medical history
presented to the emergency room with two days of tongue swelling, painful
swallowing, fever, and difficulty speaking. The patient complained of some
difficulty in breathing. Physical exam revealed moderate swelling and
tenderness of the dorsum of the tongue with a 1cm right paramedian mass just
anterior to the circumvallate papillae. Of note, there was no pigmentation
changes or ulceration reported. The patient did not have stridor.
Friday, 27 April 2018
Wrist Arthroplasty Leads to Better Outcomes than Arthrodesis for Treatment of Patients with Advanced Rheumatoid Arthritis of the Wrist: A Review of Literature
Rheumatoid arthritis is a chronic inflammatory condition of unknown a etiology, which can be disabling causing up to 35% of patients with 10 years of symptoms to early retire and carries a high mortality rate. It targets mainly the synovial membrane and articular cartilage of joints leading to joint deformity and instability. Genetic, immunological and environmental factors are thought to cause the disease in such a way that susceptible genes are triggered by infection or environmental factors leading to inappropriate immune response attacking the joints.
Around 1% of general population is affected in the UK it is estimated to affect about 0.8% of the population and in some countries, where it is prevalent, it affects about 2% of population above 60 years. Though highest rates are in north Europe and America some studies are showing decrease of incidence in these regions. It is more common in white race affecting elderly in the 5th and 6th decade with women being affected 3 folds more than men.
Wrist and hands are the most common joints affected in rheumatoid arthritis such that by 4 years of the onset of the disease more than 90% of patients would show symptoms of involvement of at least one of these joints. Affection of carpal ligaments and tendons around the wrist would lead to radial deviation of radio carpal joint with ulnar deviation of the fingers at the MCP joint, subluxation ofdistal ulna and dropped fingers resulting in a zigzag deformity or what is known as caput ulnae syndrome. Half of the patients might have systemic or extra articular manifestations (ExRA). Nodules are the most common ExRA with the cardiovascular system being the most affected and this might be the reason why these patients show a higher mortality rate than the non-ExRA subgroup. Patient presents complaining of painful, swollen, stiff joints, especially after period of rest, and even obvious deformity in late presentations. It is characterized by periods of remission and activity, which can be assessed using scores as the Disease Activity Score (DAS28).
Thursday, 26 April 2018
Effectiveness and Safety of a Combination of Intra- Articular Corticosteroid and Local Anesthetic in Indian Patients with Knee Osteoarthritis: A Pilot Study
Intra-articularcorticosteroids are often used along with local anesthetics to treat
osteoarthritis probably due to the rationale that the local anesthetic
component acts quickly after administration, to provide immediate pain relief,
and its action may last until the corticosteroid component starts to exert its
effect. While some studies suggest that a combination local
anesthetic/corticosteroid may have potential negative effects on
intra-articular cell viability and cell metabolism, and may lead to chondrotoxicity,
others support continued safe use of this combination in clinical practice.
Nonetheless the combination of intra-articular steroids and local anesthetics
is routinely administered universally (either in the same syringe or
separately) to treat osteoarthritis.
The potential advantage of rapid onset
and prolonged duration of action offered (which enables instant pain relief and
anti-inflammatory response) by combination of intra-articular steroids and
local anesthetics, as well as the controversy surrounding its safety makes it
imperative to examine its effectiveness and safety in patients with knee
osteoarthritis. However, studies exploring the effectiveness and safety of this
combination are limited especially in
India. Therefore, this pilot study was conducted to determine the effectiveness
and safety of administering a combination of intra-articular corticosteroid and
local anesthetic in Indian patients with knee osteoarthritis.
Adults between 35-70 years of age,
suffering from chronic knee pain (pain score at least 3 cm on Visual Analogue
Scale [VAS] for at least three months prior to inclusion, with a clinical or
radiological diagnosis of knee osteoarthritis, dissatisfied with previous
non-surgical management including analgesics and other drugs were included
after informed consent. Those with severe, advanced, destructive arthritis with
deformity, neuropathic or septic arthritis.
Wednesday, 25 April 2018
Emergency Contraception Editorial Commentary
http://austinpublishinggroup.com/obstetrics-gynecology/onlinefirst.php
Emergency contraception is method of contraception that helps to prevent unintended and unplanned pregnancies after unprotected sex and before the implantation. This contraceptive method includes either the use of Emergency Contraceptive Pills (ECPs) levonogestrel in a single dose 1.5mg, ulipristal acetate in a single pill containing 30mg or Copper-containing IUD s. The recommendation timeframe to use the emergency postcoital contraception is as following: levonogestrel pills should be taken within 72 hours, ulipristal acetate pills are indicated up to 120 hours and Copper-containing IUDs may be insert intrauterine up to 5-7 days after unprotected intercourse respectively. The exact mechanism of action of EC is not yet clear, but theoretically it can affect follicle maturation, ovulation process, quality of cervical mucus, fertilization, zygote development and transport. Also, the mechanism of action varies depending on the formulation, but also for the same formulation depends on the time of receipt in relation to sexual contact and ovulation.
Time range the effectiveness of emergency contraception decreases as long as the time elapses from sexual intercourse to the start of treatment. A sexual contact is considered unprotected when one of the following occurs: Failure to use a contraceptive method, Condom breaking or leakage, Displacement of contraceptive diaphragm or cervical cap, Do not intake a contraceptive pill on the 1st week, Do not intake 3 or more contraceptive pills on the 2nd or 3rd week, Do not intake a progestogen pill, Detachment of a contraceptive patch, Delay of Depo-Provera injection over 2 weeks, Ejaculation in the external genitalia, Sexual abuse of a woman who does not use a reliable contraceptive method. Contraindications There are no absolute contraindications to EC, except for pregnancy, and this is because it is effective. Recent studies have shown no teratogenic effects on the neonate or adverse outcome of pregnancy, and therefore it is not advisable to stop a possible pregnancy. Monitoring A pregnancy test should be recommended in women with no menstrual bleeding 21 days after taking EC. At the same time, a follow-up consultation may be provided for contraceptive methods and prophylactic screening for sexually transmitted diseases.
Tuesday, 24 April 2018
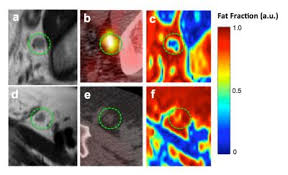
Effects of Soy Supplementation on Abdominal Obesity and Metabolic Risks on Post-Menopausal Women: A Pilot Study
http://austinpublishinggroup.com/obesity-metabolic-syndrome/
DEXA: Dual-Energy X-ray Absorptiometry;
CRP: C-Reactive Protein; IL-6: Interleukin 6; BMI: Body Mass Index; CVD: Cardiovascular
Diseases; HRT: Hormone Replacement Therapy; IRB: Institutional Review Board;
UTSA: The University of Texas at San Antonio; HDL: High-Density Lipoprotein;
LDL: Low-Density Lipoprotein; TC: Total Cholesterol; TG: Triglyceride; ELISA:
Enzyme-Linked Immunosorbent Assay; Waist: Waist Circumference; HOMA-IR:
Homeostasis Model Assessment-Insulin Resistance; GI: Gastrointestinal; SBP:
Systolic Blood Pressure; DBP: Diastolic Blood Pressure; GLM: General Linear
Model; SE: Standard Error; MRI: Magnetic Resonance Imaging; CT: Computer
Tomography; Intervention: Intervention Group; Control: Control Group.
Menopausal women are among the highest
risk populations for abdominal obesity and at great risk of developing
metabolic abnormalities. It was observed that menopausal women tend to
accumulate visceral fat, which is a key risk factor for metabolic syndrome. The
withdrawal of estrogen has negative effects on the cardiovascular system
including: the transition from a gynoid to an android adipose storage pattern,
reduced glucose tolerance, abnormal lipid profile, increased blood pressure,
increased sympathetic tone, endothelial dysfunction, and vascular inflammation.
Among the inflammatory factors, cytokine interleukin 6 (IL-6) may lead to
mediating pathways for cardiovascular diseases (CVD); while C-reactive protein
(CRP) is an indicator of metabolic abnormality and CVD in post-menopausal women.
Hormone replacement therapy (HRT) has
been shown to be effective in reducing visceral fat and improving lipid profile
in menopausal women. However, HRT may increase risk of breast and uterine
cancers. As such, prolonged use of HRT is not recommended for CVD prevention.
Therefore, safe, hormone substitute compounds exerting estrogenic properties
are warranted to prevent and treat estrogen deficiency related disease states,
e.g. abdominal obesity and its metabolic complications.
Monday, 23 April 2018
The Recognition of Respiratory Failure in Amyotrophic Lateral Sclerosis - Delays and Distress
http://austinpublishinggroup.com/austin-neurology/
Amyotrophic Lateral Sclerosis/Motor
Neurone Disease (ALS / MND) is a progressive disease of the nervous system
affecting primarily, but not exclusively, motor neurones. The cause is unknown,
but in 5-10% of cases there is a family history and there is increasing
evidence of a genetic basis for the disease, with an unknown provoking
environmental or other genetic involvement. Most people with ALS/MND
present with muscle weakness, in arms or legs, or as swallowing or speech
problems due to bulbar involvement. However a small proportion of people
present with respiratory muscle weakness often as an emergency when they
may even need ventilation, by non-invasive ventilation or invasive ventilation
with a tracheostomy.
These cases show the issues that may
arise when there is a misdiagnosis of symptoms, without a full assessment of
the person’s history, symptoms and signs. Increasingly patients may be seen as
presenting with a particular symptom complex which is considered to be related
to a particular diagnosis, without consideration of the whole patient and a
careful assessment of the situation. The names and details have been changed to
protect anonymity.
Mr M was a 70 year old man who had
suffered from heart failure since 1999 when he had undergone a coronary
arterial bypass graft. He had been seen on a regular basis by cardiology
services, including the specialist heart failure team. In September 2011 he was
seen with increasing dyspnoea, which he stated had been present for over a
year. His main symptom of waking at night was thought to be paroxysmal
nocturnal dyspnoea. At the end of January 2012 he was admitted to hospital with
shortness of breath on minimal exertion and was found to be in fast atrial
fibrillation. This was treated but the episodes continued.
Saturday, 21 April 2018
Therapeutic Use of Wheat Grass Juice for the Treatment of Anemia in Young Women of Ajmer City (Rajasthan, India)
Wheat grass juice isextracted from the cotyledons of the common wheat plant Triticum
aestivum. It has been used therapeutically from years all around the world
because of its healing properties. The juice from wheat grass is high in
chlorophyll, active enzymes, vitamins and other important nutrients like Iron. The chlorophyll present in wheat grass and haemoglobin has similar
structures except for the central moieties. Also the pH of wheat grass juice is
7.4 which are the same as that of blood. Therefore it is absorbed quickly in
the blood and is often referred to as Green Blood. This juice is extensively
used therapeutically for the management of diseases like Anemia, Thalassemia,
Inflammatory Bowel diseases, etc.
According to
the National Family Health Survey- 3, more than half of women (55 percent) aged
between 15 to 49 years are Anaemic. Nutritional deficiency anaemia refers to a
decrease in the concentration of haemoglobin in the blood due to poor dietary
habits that causes deficiency of iron, proteins, vitamins like vitamin C,
vitamin B12 along with folic acid. Deficiency of the above
nutrients can affect the production of red blood cells. Anaemia is a wide
spread public health problem which is associated with an increased risk of
morbidity and mortality. India is among the countries with the highest
prevalence of iron deficiency anemia in the world
The reduction in oxygen
available to organs and tissues when haemoglobin levels are low is responsible
for many of the symptoms experienced by anaemic people. The consequences of
anaemia include general body weakness, frequent tiredness, and lowered
resistance to disease. Anaemia can be a particularly serious problem for
pregnant women, leading to premature delivery and low birth weight. It is of
concern in children since anaemia is associated with impaired mental and
physical development. Haemoglobin testing is the primary method of Anaemia
diagnosis. Age is
associated with the category of Anaemia, with older women being somewhat more
likely to be moderately or severely anaemic than younger women. The rate of
moderate-to-severe Anaemia (moderate and severe Anaemia combined) among women
of age 35- 49 is almost three times as high as among girls of age 15-19.
Friday, 20 April 2018
Mechanisms of Twinning IX: Influence of Prior Lactation
The purpose of this study is to
ascertain a physiological relationship between prior lactation and the
probability of subsequent multiple pregnancies in humans, thereby lending
support to the role of insulin-like growth factor in both phenomena. Data were
collected in the present study to determine if there is a direct relationship
between the extent of lactation in prior pregnancies and the chance of
twin/triplet gestations subsequently. Positive results of such a study could
support the proposed biochemical significance of insulin-like growth factor
elevation in promoting multi-fetal pregnancies.
Cows with an enhanced tendency to twin
have elevated levels of serum Insulin-like
Growth Factor (IGF).
IGF is a protein component of milk; bovine milk has a lower level of IGF
than human milk, in general.
Recent reports support the view that twinning in humans is also related in some
way with IGF. Somatotropin-stimulated IGF
augmentation often induces ovarian hyperstimulation in subfertile women
undergoing in vitro fertilization. On the other hand,
one small study found no significant difference in plasma follicle stimulating
hormone (FSH) between mothers of Dizygotic (DZ) twins and mothers of singletons
at any stage of the menstrual cycle.
Insulin-like growth factor, a 70-unit polypeptide,
is a major mediator of FSH action on the
ovary.
IGF increases the sensitivity and responsiveness of ovaries to FSH. Variations
in either FSH or IGF can modify the Spontaneous
Twinning Rate (STR).
The mitogenicly powerful synergistic combination of IGF and FSH enhances
ovarian steroidogenesis, increases primordial follicle recruitment, and reduces
ovum apoptosis, thus increasing the chance for double ovulation. In
humans, conceptions that occur while the mother is breast-feeding result in
twin gestation rates (both monozygotic and dizygotic) nine times higher than in
the general gravid population. Also, women who have ever lactated have a higher
mean plasma IGF level than those who never lactated.
Human grand-multiparas (parity>4)
more often breast-feed than women
with fewer pregnancies.
Also, elderly (age>40) grand-multiparas retain their fertility longer and
conceive twins more often than
do women of low parity.
Thus, the current potential for twinning may be a function of lactation in
prior pregnancies. By its cumulative effect, prolonged lactation might extend
the period of enhanced availability of IGF.
Thursday, 19 April 2018
Development of a Comprehensive Psycho Social Care and Support Model for Children and Adolescents Living with HIV/AIDS in India
http://austinpublishinggroup.com/nursing/
Globally, it was estimated that in the
year 2008 there were 33.4 million people living with HIV, out of which children
below 15 years constituted 2.1 million. It was estimated that India has an
overall prevalence of 0.31%. Approximately 50,000 children below 15 years are
infected by HIV every year. The increased access to antiretroviral
treatment resulted in increased survival rates among the children infected with
HIV/AIDS and also led to the improved quality of life of sero-positive
children. This continues to have an increased impact on the mental health of
children and adolescents living with HIV. Children with any chronic illness, in
general, are found to be at greater risk of psychiatric problems, including
depression, anxiety, and feelings of isolation. A major factor that
distinguishes HIV/AIDS from other chronic or terminal illness is the stigma.
Too often many HIV infected children and their families live in shame
associated with AIDS.
Illness is often kept as a secret. Parents delay
disclosing child’s as well as their own HIV/AIDS illness status due to stigma
and possible psychological consequences. Internalizing problems such as
anxiety, withdrawn behaviour, depression and somatic complaints are more in
younger children with HIV and externalizing problems such as rule breaking,
aggressive behaviour, and conduct disorders are common among older adolescent
living with HIV. Further, children with HIV/AIDS have additional
factors in the complexity of their illness and treatment as well as in the
adverse psychological circumstances and poverty in which many live. These
children who know about their HIV status live in fear of their disease, and
fear of loss of parents with HIV/AIDS. Moreover, given the nature of HIV
transmission, if both parents infected with HIV, then many children become
‘double orphans’. Children not only have to endure the pain and loss of losing
parents, and also have to face stigma and survive without the emotional support
of their parents. Following the death of the parents most of these infected
children end up in living in orphan homes for long term care and protection.
This has immediate as well as longer term emotional consequences. As a
result the mental health, needs and concerns of the children and adolescents
with HIV infection need to be an essential part of their care even with
advancements in HAART.
When it comes to the disclosure of HIV/AIDS infection
status to the children, there is no clear consensus among the practitioners and
parents on when to disclose the HIV positive status to the child. Most of the
disclosure guidelines address on illness aspect and treatment adherence and not
on addressing the mental health impact of disclosure of HIV status to the child. Once the HIV diagnosis has been disclosed to the infected child, there is
a need to monitor in every follow-up visit, the child’s level of functioning,
behavioural changes, emotional and psychological adjustment by the health care
provider. Moreover, health care providers who work directly with HIV infected
children are not being trained with adequate skills to handle the psychosocial
and mental health issues of children infected with HIV/AIDS. This adds to
the woes of the children in vulnerable situations and affects their not address
the psychological and mental health issues of children either infected or
affected with HIV/AIDS. The existing services in the ART centers in India are
more generic than specific needs of infected children and adolescents.
Wednesday, 18 April 2018
Food Patterns, Diabetes and Overweight/Obesity and Some Socio-Economic Indicatorsin the Italy Regions
Thepurpose of this study is to identify the differences in mortality due to type 2
diabetes (T2D), the increase of overweight and obesity in the different regions
of Italy and their relation with change in dietary patterns within the
framework of some economic indicators. In Italy in 2015, the
total adult population (1000s) (20-79 years) were 44,704; the prevalence of
diabetes in adults (20-79 years) was 7.9%. The number of deaths in adults due
to this disease was 22,226. Cost per person with diabetes (USD) was 3,450.1.
The number of undiagnosed cases of this disease in adults was (1000s) 1,324.3.
According to the International Diabetes
Federation (IDF) the overall prevalence of T2D in 2015 was 8.8%, of which
approximately 75% were people living in low and middle-income countries. The
fastest increase of cases occurred in regions where the economy moved from low
to middle-income. In low and middle-income regions, the number of people with
diabetes will increase 150% over the next 25 years. Moreover, 318 million
people live with impaired glucose worldwide. The IDF calculated that in the same
year about 46.5% (193 million) patients were undiagnosed worldwide and one in
seven births was affected by gestational diabetes. The disease caused 5 million
deaths and resulting in 673 billion
dollars being spent on care.
In
2015, 415 million people had diabetes worldwide. More than 59.8 million of
those were in the EUR Region and over 3.5 million cases (adults 20-79 years)
were in Italy. In this regard, structural social
determinants should be considered, covering a wide and complex combination of
socio-economic conditions and interacting cultural and other environmental
elements. The conditions in which the population is born, grows, lives, works,
and ages, as well as the type of systems used to combat the disease are those
that determine inequality and social inequity. Political and economic forces in
each region in turn influence these conditions. Analysis of health problems
using social determinants is a framework of reference for research in various
areas of public health and epidemiology. The field of knowledge and purpose of
the DSS is to analyze inequities in the distribution of social goods and how
avoidable inequalities are manifested in the state of health of social groups. Economic
development has led to greater availability and diversity of the food in almost
all countries and a gradual decree in food shortages, resulting in nutritional
condition. There have also been improved living standards and increased access
to services. However, these improvements differ between countries with low,
medium and high income and between population groups within each country.
Tuesday, 17 April 2018
Monogenic, Polygenic and Multifactorial Obesity in Children: Genetic and Environmental Factors
http://austinpublishinggroup.com/nutrition-metabolism/
Obesity is achronic disease that has increased alarmingly in recent years. It is considered
a risk factor for the development of diseases such as type 2 diabetes,
cardiovascular diseases, dyslipidemia, and some types of cancer. Two genetic
profiles have been described: monogenic obesity, in which a single gene is
mutated, usually leading to loss-of-function or haploinsufficiency, and
polygenic obesity, which involves several polymorphic genes with complex
interactions between genes and environmental factors. In the latter case, the
frequency of polymorphisms can be very high, depending on the population
analyzed. In both cases, the genes of interest are associated with changes in
body composition through different mechanisms, including hyperphagia, energy
expenditure, adipocyte differentiation and lipolysis. However, most studies
have analyzed genes associated with obesity in other populations, and the results
are often inconsistent, so it is important to study the context of obesity,
such as genetics, biochemical biomarkers and environmental factors.
Environmental factors include physical activity, nutritional status, and an
intake of foods rich in fats and carbohydrates that favor obesity in children.
In addition, several chemical compounds have been described as potential
endocrine disruptors that increase BMI and produce obesity, and some biological
agents can alter the homeostasis of adipose tissue. In this review, we analyzed
the genetic and environmental factors that influence obesity, particularly in
children.
OECD: Organization for Economic
Cooperation and Development; BMI: Body Measured Index; LEP: Leptin; LEPR:
Leptin Receptor; POMC: Proopiomelanocortin; PCSK1: Prohormone convertase 1/3;
MC4R: Melanocortin 4 Receptor; SIM1: Single Minded Homologue 1; GWAS: Genome
Wide Association Studies; PPARG: Peroxixome Proliferator-Activated Receptor γ;
ADIPOQ: Adiponectin; FTO: Fat-Mass and Obesity Associated Gene; SNP: Single Nucleotide
Polymorphism; CED: Chemical Endocrine Disrupters; DDE:
Diphenyl-dichloro-Ethylene (DDE); BPA: Bisphenol A.
Obesity is a chronic disease of diverse
etiology. In the genetic context, monogenic obesity is associated with
loss-of-function mutations in a single gene. These mutations are very rare and
are in some cases unique to a patient or several members of a family; in some
populations with high rates of consanguinity, the mutations are more frequent. In polygenic obesity, there is an interaction between several polymorphic
genes; in this case, the frequency is greater than 1% and varies by the
population analyzed. In this type of obesity, the risk that is attributed to
each allele is generally small, but the additive effect of several risk alleles
can considerably increase susceptibility to obesity.
Monday, 16 April 2018
An Impact of Pelvic Magnetic Resonance Imaging to Radiotherapy Volume Definition in Patients with Intermediate- and High-Risk Prostate Cancer: A Population Based Study
Pelvic MRI (PMRI)
is an important pre-radiotherapy (RT) evaluation procedure in patients with
intermediate- and high-risk prostate cancer. We conducted a retrospective study
to evaluate an influence of PMRI to delineation of RT clinical target volume
(CTV).
Medical records of
prostate cancer patients treated with intensity-modulated RT (IMRT) in single
institution in 2009-2015 were retrieved and examined retrospectively. Initial
risk group affiliation was defined using NCCN criteria. PMRI reports of
patients with intermediate and high-risk prostate cancer were reviewed and risk
group affiliation was re-defined in regards of T- and N-stage. CTVs for IMRT
treatment plans were contoured. Accounting to information obtained from PMRI.
Extra-capsular extension (ECE) and seminal vesicles invasion (SVI) were
included to high-dose CTV. Regional pelvic lymph nodes (RPLN) were planned to
treat in all high-risk pts. RPLN considered pathological by PMRI were included
to separate CTV to receive RT dose higher than unaffected RPLN stations.
Between 2009 and
2013, 169 patients with intermediate and high-risk prostate cancer underwent
PMRI at around 1 month before commencing IMRT. Initially, 89 patients were
affiliated to intermediate-risk and 80 to high-risk group. In general,
PTV-changes based on PMRI data required in 66 patients (39%). Thirty seven of
89 intermediate-risk patients (42%) were switched to high-risk group,
necessitating irradiation of RPLN. ECE and SVI were included to high-dose CTV
in 64 (38%) and 29 patients (17%) respectively. RPLN were thought pathological
in 10 patients (6%), which justified contouring of a separate CTV for dose
escalation.
In our retrospective
series, PMRI-scans had a significant impact on RT target coverage decision in
patients with intermediate and high-risk prostate cancer. However, a true value
of this impact should be defined a large scale prospective clinical trial.
Friday, 13 April 2018
Whistleblower Issue and Its Relevance in Autism Research
On August 27, 2014, CDC
scientist Dr. William Thompson admitted that he and other authors had omitted
vital data from a 2004 study of possible connections between MMR vaccines and autism.
Dr. Thompson also acknowledged a biologically plausible relationship between
Thimerosal (a mercury-based preservative) in vaccines and autistic-like
symptoms. He additionally reported that the CDC has withheld information about
a relationship between Thimerosal and tic disorders. Whether or not a person
thinks that the admissions made by this CDC scientist reflect the truth,
admitting fraud in the CDC's neurodevelopmental disorders research is certainly
newsworthy. Why then has the mainstream media been mostly silent on the issue?
The coverage of this story has been mostly limited to the blogosphere. Some of
the mainstream media's top stories have instead included: "Artists draws
his dog in whimsical scenes" (ABC News, 9/17/14); "Is the tide
changing for the NFL" (MSNBC, 9/17/2014); and "Vikings: Peterson must
stay away", and "Final hours before Scotland's big vote" (CNN,
9/17/14).
Admittedly,
this CDC whistleblower story is controversial. This is due, in part, to
enormous and far-reaching liability ramifications, to the disturbing number of
potentially affected children, and because those that could be held accountable
hold powerful and authoritative governmental positions. We can only speculate
if the mainstream media is simply not interested in this topic, or if their
silence reflects a form of disagreement, or if possibly their lack of coverage
is due to external pressure to extinguish the story. The limited mainstream
media coverage of such a weighty scientific matter reveals the importance of
scientists themselves having a public voice on critical public policy issues.
Throughout history scientists speaking loudly about dangerous toxins have saved
many lives and prevented untold pain and deformities. Clear examples are Pink
disease (caused by mercury in teething powders), lead poisoning diseases (from
lead-based paints and other products), and thalidomide causing birth defects. And
also, of course, the discovery that mercury causes neurological damage. The
mainstream media's silence here emphasizes the value of peer-reviewed science
journals as an avenue for scientists to be a part of necessary public
dialogues.
This story also raises
the issue of the importance of transparency in research and the availability of
public databases to independent researchers. The current datasets used by the
CDC in their own research on vaccines and autism are not easily accessible to
independent researchers. For example, one of the databases used by the CDC that
reportedly showed no relationship between thimerosal and autism is no longer available to anyone outside of
the CDC to examine. Neuropsychiatric disorder research data transparency is
especially important considering today's staggering numbers of
neurodevelopmental disorders, which in the United States has increased to about
1 in every 6 children. This has predominately been an increase in autism and
attention deficit/ hyperactivity disorders, but there has also been an increase
in tic disorders. World-wide neuro developmental disorders today are causing
heavy consequences on the affected individuals and their families. How this
unfolds remains to be seen. However, assuming continued mainstream media
silence, it is likely that this whistleblower story along with its potential
implications will remain missing from the forefront of public discussion.
Thursday, 12 April 2018
Transcriptome Analysis of Rotenone Induced Neurotoxicity in Enriched Rat Primary Ventral Mesencephalic Neurons
http://austinpublishinggroup.com/neurology-neurosciences/
Rotenone induced neurotoxicity is being
widely investigated in relation to Parkinson’s Disease (PD). However the
crucial molecular mechanisms involved in rotenone induced PD still remains
elusive. This report details the transcriptome changes on rotenone treatment in
enriched rat primary ventral mesencephalic neurons through microarray analysis.
Transcriptome analysis had yielded 705 up-regulated genes and 2415
down-regulated genes. This data was further validated by quantitative real time
PCR analysis. To further refine this data, association rule mining was used and
a gene interaction network among 53 genes was developed. Functional characterization
of the top 25 scored genes in the network was done using panther database.
Interestingly TNF was the highest scored gene among them and found to be
significantly down regulated on rotenone treatment. Along with TNF other
inflammation related genes like Il1b, Itpr3 and TNFR2 were also significantly
down-regulated on rotenone treatment. These observations suggest that down
regulation of neuronal TNF might be a critical cause leading to cellular death via
TNFR2, Il1b mediated Pi3Kinase pathway in rotenone induced neurotoxicity.
Further investigation in this neuronal TNF related pathways may give novel
therapeutic approaches in treatment of PD.
In-Vitro/In-Vivo treatments with
rotenone are known to induce certain features of Parkinson Disease (PD).
Dopaminergic neurodegeneration in substantianigra pars compacta of Ventral
Mesencephalic (VM) brain region is the hall mark feature of PD. Rotenone,
besides affecting mitochondrial function was also reported to be affecting a
variety of cellular processes like cytoskeleton stability, inflammation,
oxidative stress and apoptosis. All these observations were made using
directed approaches studying few of the genes involved in those specific
pathways. Microarray analysis of whole transcriptome is an alternative approach
for identifying key genes and pathways that might not be feasible through
single-gene studies. Enriched rat primary VM neurons were well characterized and studied in co-relation with rotenone induced neurotoxicity. In the
present study primary VM neurons were analyzed for changes in their genome
expression upon rotenone treatment using microarray analysis along with Association
Rule Mining (ARM) for discovering the relationship among genes in a large
dataset.
Wednesday, 11 April 2018
Spinal Cord Injury Intensity Modifies the Expression of Inflammation-Related Gene Expression after Immunization with Neural Derived Peptides
Previous
studies revealed that the intensity of Spinal Cord Injury (SCI) plays a key
role in the therapeutic effects induced by Immunizing With Neural-Derived
Peptides (INDP), as severe injuries abolish the beneficial effects induced by
INDP. In the present study, we analyzed the expression of some
inflammation-related genes (IL6, IL12, IL-1β, IFNɣ, TNFα, IL-10, IL-4, and
IGF-1) by quantitative PCR in rats subjected to SCI and INDP. We investigated
the expression of these genes after a moderate or severe contusion. In
addition, we evaluated the effect of INDP by utilizing2 different peptides: A91
and Cop-1. After moderate injury, both A91 andCop-1 eliciteda pattern of genes
characterized by a significant reduction of IL6, IL1β,andTNFα but an increase
in IL10, IL4, and IGF-1expression. There was no effect on IL-12 and INFɣ. In
contrast, the opposite pattern was observed when rats were subjected to a
severe spinal cord contusion. Immunization with either peptide caused a
significant increase in the expression of IL-12, IL-1β, IFNɣ, (pro-inflammatory
genes), and IGF-1. There was no effect on IL-4 and IL-10 compared to controls.
After a moderate SCI, IND Preduced pro-inflammatory gene expression, and
generated a microenvironment prone to neuroprotection. Nevertheless, severe
injury elicits the expression of pro-inflammatory genes that could be
aggravated by INDP. These findings correlate with our previous results
demonstrating that severe injury inhibits the beneficial effects of protective
autoimmunity.
Tuesday, 10 April 2018
Approach to Imaging in Mild Traumatic Brain Injury and Diffuse Axonal Injury
http://austinpublishinggroup.com/neurosurgery/onlinefirst.php
Traumatic brain injury is a commonly
encountered condition in the emergency department. Mild traumatic brain injury
and its squeal of diffuse axonal injury are difficult to diagnose with computed
tomography scans as the preferred acute imaging modality. Our current decision
on whether or not to scan a patient in the acute setting is best decided upon
by the Canadian CT Head Rule. The role for MRI scans in diagnosing diffuse
axonal injury is unclear, but current evidence suggests that they are preferred
after the initial 48 hour period following head trauma.
While the
definition has varied depending on circumstances, Traumatic Brain Injury (TBI)
is defined as the result of the application of either external physical force
or rapid acceleration/deceleration forces that disrupts brain function as
manifested by immediately apparent impairments in cognitive or physical
function. This is further classified as mild, moderate, and severe, depending
on the patient’s Glasgow Coma Scale Score (GCS). The majority of these cases
present to hospital as minor TBI, and previous studies suggest that 40% of
these cases are secondary to motor-vehicle-related events.
In terms of neuroimaging
following head injury, the decision on whether or not to scan tends to be
guided by hospital-specific protocol, or is physician dependent. The general
consensus, however, is that patients with new clinical symptoms or a change in
GCS following head injury, should undergo a Computed Tomography (CT) scan of
the brain. The specific clinical predictors for this are still very much
debateable. The Canadian CT Head Rule study, as demonstrated in (Table 1), has
developed a highly sensitive clinical decision rule for the use of CT in patients
with minor head injuries. These patients are classified into whether or not
imaging is required based off five high-risk factors for neurosurgical
intervention, and two medium-risk factors for clinically important lesions. The
implementation of this guideline in other centres was associated with a modest
reduction in CT use and an increased diagnostic yield of head CTs for trauma to
the head.
Monday, 9 April 2018
What we do and do not know about Women and Kidney Diseases; Questions Unanswered and Answers Unquestioned: Reflection on World Kidney Day and International Woman’s Day
Chronic KidneyDisease affects approximately 10% of the world’s adult population: it is within
the top 20 causes of death worldwide, and its impact on patients and their
families can be devastating. World Kidney Day and International Women’s Day in
2018 coincide, thus offering an opportunity to reflect on the importance of
women’s health and specifically their kidney health, on the community, and the
next generations, as well as to strive to be more curious about the unique
aspects of kidney disease in women so that we may apply those learnings more
broadly.
Girls and women,
who make up approximately 50% of the world’s population, are important
contributors to society and their families. Gender differences continue to
exist around the world in access to education, medical care, and participation
in clinical studies. Pregnancy is a unique state for women, offering an
opportunity for diagnosis of kidney disease, but also a state where acute and
chronic kidney diseases may manifest, and which may impact future generations
with respect to kidney health. There are various autoimmune and other
conditions that are more likely to impact women with profound consequences for
child bearing, and on the fetus. Women have different complications on dialysis
than men, and are more likely to be donors than recipients of kidney transplants.In this editorial,
we focus on what we do and do not know about women, kidney health, and kidney
disease, and what we might learn in the future to improve outcomes worldwide.
Chronic Kidney
Disease (CKD) affects approximately 10% of the world’s adult population: it is
within the top 20 causes of death worldwide and its impact on patients and
their families can be devastating. World Kidney Day and International Women’s
Day in 2018 coincide, thus offering an opportunity to reflect on the importance
of women’s health and specifically their kidney health, on the community, and
the next generations; as well as to strive to be more curious about the unique
aspects of kidney disease in women, so that we may apply those learnings more
broadly.
Girls and women, who make up approximately 50% of the world’s
population, are important contributors to society and their families. Besides
childbearing, women are essential in childrearing and contribute to sustaining
family and community health. Women in the 21st century continue to strive for
equity in business, commerce, and professional endeavours, while recognizing
that in many situations, equity does not exist. In various locations around the
world, access to education and medical care is not equitable amongst men and
women; women remain under-represented in many clinical research studies,
thus limiting the evidence base on which to make
recommendations to ensure best outcomes (Figure 1). In this editorial,
we focus on what we do and do not know about women’s kidney health and kidney
disease, and what we might learn in the future to improve outcomes for all.
Thursday, 5 April 2018
Nanotechnology- A Promising Approach for Suicide Gene Therapy
Canceris one of the world’s most dreadful diseases and the battle against cancer
continues till date. Suicide gene therapy for cancer is one of the best
approaches for annihilation of cancer. In brief, suicide gene codes for an
enzyme which converts a nontoxic prodrug into toxic metabolites and
subsequently mediates death of host cells itself on account of which it is
named “suicide” gene therapy. These suicide gene when constitutively
expressed by the cells not only mediates death of host cells but also inflicts
strong bystander effects on neighboring cells by predisposing them to toxic
downstream metabolites. Due to such advantages, they manifest minimal systemic
toxicity and are also effective against many drug resistance cancer cells. Among
all existing suicide genes, Cytosine Deaminase (CD) and Herpes Simplex
Virus-thymidine kinase (HSVtk) have shown promising results initially and has
been investigated extensively since long. The HSVtk enzyme initially
phosphorylates the prodrug Ganciclovir (GCV) to its monophosphate form, which
is subsequently phosphorylated again by endogenous cellular kinase to generate
nucleotide analogs (di- and triphosphate forms of GVC). Triphosphate form of
GCV is then readily incorporated into DNA during the course of DNA synthesis
and acts as a chain terminator to prevent further DNA synthesis, which
ultimately induces cell death.
The
therapeutic efficacy of HSVtk suicide gene therapy is often limited by
cell-to-cell contact which is a prerequisite for transport of downstream
metabolic byproducts of ganciclovir to neighboring cells so as to attain
bystander-killing effect. As an outcome of such drawbacks, HSVtk suicide gene
does not seem to be effective against different cell types. In contrary to
this, Cytosine Deaminase (CD) efficiently converts prodrug 5-Fluorocytosine (5-
FC) into therapeutically active anticancer agent 5-Fluorouracil (5- FU), which
subsequently permeates across the cell membrane to mediate bystander killing
effects on adjacent neighboring cells. Thus, 5-FC/CD system attains suicide
gene therapy much more efficiently as compared to other counterparts. Although
5-FC/CD system attains better therapeutic outcomes, it is ineffective against
5-FC resistant cancer cells and thus its anticancer potential could not be
generalized for all cancer types. In order to overcome such drawback, Gopinath
et al. have designed Cytosine Deaminase-Uracil Phosphoribosyltransferase
(CD-UPRT) bifunctional suicide gene construct in which Uracil
Phosphoribosyltransferase (UPRT) acts upon product of CD i.e. 5-FU and converts
it further into other toxic metabolites.
The
therapeutic effect of suicide genes can be enhanced by combinatorial
approaches. In combination therapy, two or more drugs with similar or different
mode of action are employed to realize synergistic anticancer therapeutic
potentials. Such synergistic anticancer potential of combination of radiation
therapy and 5-FC/ CD plus UPRT gene therapy was demonstrated by Kambara et al.
against malignant gliomas. Apart from this, the combination therapy also
provides scope for exploiting radio sensitizing properties of 5-FU and by
stander effects during the course of treatment. Many research groups
have reported the use of suicide gene in combination with chemotherapy and
radiation to enhance the therapeutic effect and to overcome the drug
resistance. Gopinath et al. were the first to report the applications of silver
nanoparticles for synergizing the therapeutic effect of suicide gene. They
have also reported the synergistic therapeutic effect of suicide gene with
anticancer drug curcumin. One of the major challenging tasks in suicide gene
therapy is lack of suitable vectors for targeted delivery of suicide gene to
cancer cells. The application of such DNAbased therapeutics is largely limited
due to poor cellular uptake, degradation by serum nucleases and rapid renal
clearance following systemic administration. In addition to these, organ
specific targeted DNA therapy has been a major challenge to overcome off-target
gene therapy. In order to circumvent these limitations, numerous organ specific
targeted nanocarriers have been developed recently for systemic administration.
Wednesday, 4 April 2018
Obesity and Kidney Disease: Hidden Consequences of the Epidemic
Obesity has become aworldwide epidemic, and its prevalence has been projected to grow by 40% in the
next decade. This increasing prevalence has implications for the risk of
diabetes, cardiovascular disease and also for Chronic Kidney Disease. A high
body mass index is one of the strongest risk factors for new-onset Chronic
Kidney Disease. In individuals affected by obesity, a compensatory hyper filtration
occurs to meet the heightened metabolic demands of the increased body weight.
The increase in intraglomerular pressure can damage the kidneys and raise the
risk of developing Chronic Kidney Disease in the long-term. The incidence of
obesity-related glomerulopathy has increased ten-fold in recent years. Obesity
has also been shown to be a risk factor for nephrolithiasis, and for a number
of malignancies including kidney cancer. This year the World Kidney Day
promotes education on the harmful consequences of obesity and its association
with kidney disease, advocating healthy lifestyle and health policy measures
that make preventive behaviors an affordable option.
In 2014, over 600
million adults worldwide, 18 years and older, were obese. Obesity is a potent
risk factor for the development of kidney disease. It increases the risk of
developing major risk factors for Chronic Kidney Disease (CKD), like diabetes
and hypertension, and it has a direct impact on the development of CKD and its
progression to End-Stage Renal Disease (ESRD). In individuals affected by
obesity, a (likely) compensatory mechanism of hyper filtration occurs to meet
the heightened metabolic demands of the increased body weight. The increase in
intraglomerular pressure can damage the kidney structure and raise the risk of
developing CKD in the long-term.
The good news is
that obesity, as well as the related CKD, are largely preventable. Education
and awareness of the risks of obesity and a healthy lifestyle, including proper
nutrition and exercise, can dramatically help in preventing obesity and kidney
disease. This article reviews the association of obesity with kidney disease on
the occasion of the 2017 World Kidney Day.
Subscribe to:
Comments (Atom)
TB Treatment Success Rate in Ethiopia: Key Findings & Challenges
Tuberculosis (TB) remains a major global health issue , infecting one-third of the world's population . Despite efforts, Ethiopia's...
-
https://www.austinpublishinggroup.com/pediatric-oncology/ Within the most current concepts o...
-
Tuberculosis (TB) remains a major global health issue , infecting one-third of the world's population . Despite efforts, Ethiopia's...
-
https://www.austinpublishinggroup.com/urology/ Patientswith Lower Urinary Tr...