http://austinpublishinggroup.com/gastrointestinal-cancer/currentissue.php
Schwannomas arebenign tumors that arise from Schwann cells of peripheral nerve myelin sheaths.
Initially reported in 1988 by Daimaru et al. Gastrointestinal schwannomas have
an excellent prognosis after surgical resection. Patients with periportal
schwannomas can present with abdominal pain or concerning features such as
weight loss, jaundice or anorexia raising suspicion for a malignant tumor.
Schwannomas characteristically undergo cystic degeneration due to vascular thrombosis
and subsequent necrosis. Computed Tomography (CT) scan shows a well-defined,
hypodense, heterogeneous mass with peripheral enhancement making the
differentiation from a malignant tumor even more difficult. Only 15 cases of
periportal schwannomas have been described in the literature, and preoperative
diagnoses could not be made in any of them. All of these patients underwent
open surgical resection.
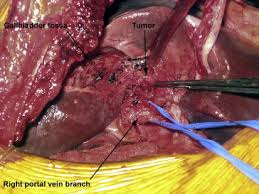
We present two
cases of periportal schwannomas approached laparoscopically. The first patient
underwent laparoscopic resection of a periportal schwannoma arising from the
proper hepatic artery. To our knowledge, this is the first reported case of
laparoscopic resection of periportal schwannoma. The second patient underwent a
diagnostic laparoscopy, and the periportal mass was confirmed as a benign
schwannoma by intraoperative frozen section. The tumor was encased around the
extrahepatic biliary tree, so it was left in-situ to avoid unnecessary
extensive biliary surgery. 55-year-old Caucasian female presented with six
months of severe abdominal pain, early satiety, bloating, steatorrhea and a
fifteen-pound weight loss. Past surgical history was significant for
laparoscopic cholecystectomy. Her laboratory studies (complete blood count,
liver function test) and tumor markers including Carcino Embryonic Antigen
(CEA) and Cancer Antigen 19-9 (CA 19-9) were within normal limit. Both upper
and lower endoscopies were normal. Abdominal CT showed a 5cm well-defined
hypodense mass in the porta hepatis (Figure 1a). No enlarged hilar lymph nodes
were identified. This was confirmed on an MRI as a 5cm complex, septated cystic
mass, hyperintense on T2 signal, adjacent to porta hepatis but separate from
the pancreas and biliary tree.
There was no intra or extra-hepatic bile duct
dilatation. A decision was made to pursue laparoscopic resection of the
periportal mass based on the extent to which the symptoms affected the
patient’s quality of life. Intraperitoneal access was gained through a Hasson
cannula and abdomen was insufflated with CO2 pneumoperitoneum to a pressure
of 12mmHg. Four 5-mm trocars were placed in the upper abdomen. After
introduction of the laparoscope (KARL STORZ, Tuttlingen, Germany), the mass was
easily identified posterior to the hepatic artery. It was
dissected carefully from surrounding structures using an ultrasonic dissector
(SonoSurg, Olympus, Tokyo, Japan). A network of peripheral nerves was seen to
be entering the tumor. The mass appeared to arise from the proper hepatic
artery. The cystic duct stump from prior cholecystectomy was identified by the
presence of surgical clips . An intraoperative cholangiogram (IOC) through the
cystic duct demonstrated normal filling of the bile duct and no communication
with the periportal mass.


No comments:
Post a Comment